Q1. What is Angina pectoris?
Ans: ANTIANGINAL DRUGS
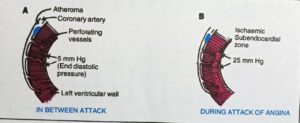
Angina pectoris is the chief symptom of ischaemic heart disease (IHD) characterized by sudden, severe, substernal discomfort or pain which may radiate to the left shoulder and along the flexor surface of the left arm, Myocardial oxygen consumption is mainly determined by preload (venous return and stretching of the heart), after load (peripheral arterial resistance) and heart rate.
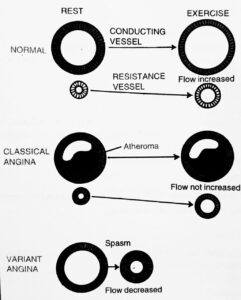
The heart normally extracts almost all the available oxygen from blood, hence the heart must therefore meet its increased metabolic demands for oxygen (in exercise or stress) by increasing the rate of coronary blood flow.
Angina is caused by the coronary vessel constriction which prevents this increase in blood flow. Reflex vasospasm of coronary arteries appears to be a primary cause of angina and it may be (but is not necessarily) superimposed on atherosclerotic coronary artery disease.
Breathlessness sometimes occurs along with other discomforts. Antianginal agents may improve angina by reducing the demand for or by increasing the supply of oxygen and dilate coronary arteries and after load (blood pressure).
Q2. Write a shot note on Types of Angina. Ans:
TYPES OF ANGINA
There are several types of angina:
- Stable angina
It is relieved by rest. chest pain precipitatel by sexcertion or stress
- Unstable angina
It is a change in the usual pattern of stable angina or a new severe angina that means blood flow has decreased.
- Angina caused by coronary artery spasms
. Most of the time coronary artery disease is involved, although sometimes plaque is not present.
- Variant angina
It also called Prinzmetal’s angina or vasospastic angina, is caused by coronary artery spasm. However, it has a distinctive pattern. It usually occurs when you are at rest and without apparent cause. The spasm often occurs at the site of coronary artery narrowing from plaque, although it can also occur in healthy coronary arteries. Variant angina episodes typically last 2 to 5 minutes and quickly subside with nitroglycerin.
Mechanism of action of antianginal drugs
These agents cause redistribution of coronary blood flow to the ischemic regions of the heart and also reduce myocardial oxygen demand. This latter effect is produced by a reduction in venous tone due to vasodilation effect and a pulling of blood in the peripheral veins that results in a reduction in ventricular volume, stroke volume and cardiac output. It also causes reduction in peripheral resistance during myocardial contractions. The combined vasodilatory effects cause decrease in cardiac workload and reduction in oxygen consumption or demand.
Q3. Write a short note on Antianginal drugs.
CLASSIFICATION OF ANTIANGINAL DRUGS
1.Nitrates
A.Short acting
- Glyceryl trinitrate (GTN, Nitroglycerine)
B. Long acting
a.Isosorbide dinitrate (short acting by sublingual route)
b.Isosorbide mononitrate, č. Erythrityl tetranitrate d.Penta erythritol tetranitrate.
2.ß-Blockers
- Propranolol b. Metoprolol c. Atenolol
3.Calcium channel blockers
- Phenyl alkylamine:Verapamil
- Benzothiazepine: Diltiazem
- Dihydropyridines:- a. Nifedipine b. Felodipine
- Nitrendipine. d. Nimodipine
- Amlodipine f. Lacidipine.
4.Potassium channel opener: Nicorandil
5.Others
- Dipyridamole b. Trimetazidine
Clinical Classification
- Used to abort or terminate attack :GTN, Isosorbide dinitrate (sublingually). B
- . Used for chronic prophylaxis :All other drugs.
- Short acting
a.Nitroglycerine (glyceryl Trinitrate)
Nitroglycerine is most commonly used nitrate successfully given in the treatment of angina pectoris. It relaxes smooth muscles throughout the body. In the vascular system it chiefly acts on the systemic veins and the large coronary arteries. Nitroglycerine primary acts on vein and causes an increases in the venous capacitances leading to a decrease return of blood to the heart which resulted in a decrease left ventricular diastolic pressure and causes a decreased myocardial oxygen requirement at rest.
Pharmacokinetics
Following a single dose, the plasma concentration of nitroglycerine reaches at peak within 2 hours which is maintained over 24 hours. The drug is mainly metabolized in the liver by a glutathione dependent organic nitrate reductase.
Adverse effect
Nitroglycerine in higher doses generally causes head ache skin rashes, postural hypotension tachycardia gastro intestinal problems nausea, vomiting etc.
Preparation and dose
Nitroglycerine (Angised) is available in 0.3 mg. 0.4 mg and 0.6 mg of tablets
Dose:0.2-0.6 mg sublingually
B.Long acting
a.Isosorbide dinitrate
Sorbitrate affects the pre-load and the post-load which is the main factor of its action on myocardial oxygen consumption. It also exerts a motor activity on the coronary vessels and on the myocardialfunctions. The drug also improves the cardiac performance and ensures better perfusion of the drug.
Pharmacokinetics
The drug is nearly completely absorbed by the body. It has a half life of about 40 minutes. The drug under goes biotransformation and the two main metabolites are isosorbide-5-mononitrate and isosorbide-2-mononitrate and these two metabolites posses powerful activity with biological half life of about 4 to 5 hours.
Preparation
Isosorbide digitate is available in tablets which are given sublingually, orally and in chewable form.
Dose
Sublingually the dose is 2.5 – 10 mg every 2-4 hours orally, the dose is 10-60 mg every 4-6 hours. In chewable form the dose is 5-10 mg every 2-4 hours.
b.Isosorbide mononitrate (Monotrate)
It an active metabolite of isosorbide dinitrate which does not undergo first pass metabolism. It has better bioavailability, less individual variation and has longer duration of action.
- B-blockers
These drugs are one of the important groups of drugs for chronic stable angina. Beta-blockers in therapeutic doses reduce the frequency of anginal episodes and raise the anginal threshold when given alone and in combination with other antianginal agents.
Mechanism of Anti anginal Action
Beta-adrenoceptor blockers reduce myocardial oxygen demand by their ability to attenuate cardiac responses to adrenergic stimulation especially increases in heart rate and contractility. Thus beta-blockers reduce myocardial oxygen demands during activity or excitement when increased sympathetic activity occurs. During rest; the effects on heart rate and myocardial contractility, though significant, are less pronounced because of lower adrenergic drive to the heart in the basal state. Beta-blockers also lower myocardial oxygen demand by reducing arterial pressure and are extremely useful antihypertensive agent.
Pharmacological actions
Exercise and emotional excitement induce angina in susceptible subjects by the increase in heart rate blood pressure, myocardial contractility and oxidative metabolism, which they cause through increased sympathetic activity. Beta-receptor blocking agents prevent angina by blocking all these effects. Moreover, they help to control hypertension in hypertensive patients in the resting state as well.
Adverse reactions
The important adverse reactions of relevance to antianginal therapy are:
- Precipitation or aggravation of congestive heart failure: Patients receiving both digoxin and a beta-blocker should be watched for the development of heart block.
- Development of severe syncope on using NTG or amylnitrite in patients on a beta-blocker..
Doses
a.Propranolol: 10-40 mg three times a day.
b. Metaprolol: 50-200 mg daily in divided doses.
c. Atenolol: 50-100 mg once a day.
3.Calcium channel blockers
Calcium is necessary for the excitation-contraction coupling in both the skeletal and smooth muscle. However, in contrast to the contractile activity of the skeletal muscle, the contractility of the cardiac and vascular muscle is highly dependent on the extracellular calcium concentration,
Types of calcium channel
Three types of Ca* channels have been described in smooth muscles (other excitable cells as well):
a.Voltage sensitive channel
Activated when membrane potential drops to around -40 mV or lower.
b. Receptor operated channel
Activated by Adr and other agonists-independent of membrane depolarization (NA contracts even depolarized aortic smooth muscle by promoting influx of Ca** through this channel and releasing Ca** from sarcoplasmic reticulum).
c. Leak Channel
Small amounts of Ca** leak into the resting cell and are pumped out by Ca**ATPase.
Pharmacological action
1.On smooth muscles
All types of smooth muscles, the resting tone and contractile responses are dependent on transmembrane calcium influx. Calcium channel blockers cause relaxation of smooth muscles. Vascular smooth muscle appears to be more sensitive but other smooth muscles like bronchiolar, gastrointestinal and uterine are also relaxed. On the vascular system, the arterioles are more sensitive than the veins so postural hypotension is not a real problem. Blood pressure is reduced especially with nifedipine. Vascular resistance is reduced and so is the coronary artery tone.
2.On cardiac muscle
Cardiac muscle is highly dependent on calcium influx for normal function. Calcium channel blockers reduce cardiac contractility and cardiac output in a dose dependent fashion. The cardiac output may also be decreased, thereby, reducing the oxygen requirement of the myocardium.
3.Antiarrhythmic action
Verapamil is very potent in this respect. Calcium channel blockers decrease the rate of discharge of SA node, suppress ectopic pacemaker activity, increase the refractoriness of the AV node and slow the conduction of a propagated impulse in the heart muscle. This effect plus the reduction of cardiac ischaemia (by decreasing O,
consumption) account for the potent antiarrhythmic action of verapamil.
4.On coronary arteries
These drugs are more potent than glyceryl trinitrate as coronary artery dilators. Calcium channel antagonists dilate both large and small branches while glyceryl trinitrate dilates only the big branches. These drugs are, therefore, more effective in “variant angina” or Prinzmetal’s angina.
Pharmacokinetics
CCBs are well-absorbed but undergo extensive first pass metabolism. They are all highly plasma protein bound and are metabolized in the liver.
Adverse effects of calcium channel blockers
Excessive inhibition of calcium influx can cardiac repression including cardiac arrest, bradycardia, AV block and congestive heart failure. However, these effects are rare. Minor side effects such as flushing, oedema, dizziness, gingival hyperplasia, nausea and constipation are also reported.
Uses of calcium channel blockers
a. Cardiovascular
- 1.Prinzmetal’s variant angina
- Stable angina pectoris
- Unstable angina
- Silent myocardial ischaemia
- MI
- Atrial fibrillation and flutter
- Paroxysmal supra ventricular tachycardia
- Systemic hypertension
- Anti atherogenic properties (decreased calcium accumulation within arterial wall cells).
b.Non cardiovascular
- Neurological disorders (nimodipine and flunarizine have been tried use limited.
- Migraine prophylaxis (well established)
- Epilepsy (flunarizine reduces seizures not responding to conventional therapy)
- Vertigo (beneficial effects of cinnarizine a selective calcium channel blocker).
Drugs
Verapamil
Dose 40-80 mg by the oral route. Intravenous dose: 5 mg. Side effects are bradycardia and hypotension.
Nifedipine (calcigard)
It is more potent than verapamil . Side effects are headache, flushing and GIT intolerance. Dose: 10-20 mg three times a day.
Diltiazem
Useful both as a prophylactic and in treatment of angina. Dose: 50 mg 3 times a day as tablets and sustained released capsules.
Nicardipine:
Dose 20-40 mg 3 times a day as tablets.
Nimodipine
: Dose 60 mg/4 hourly for 21 days.
- Potassium channel Opener
The group includes: diazoxide and minoxidil used in hypertension; and nicora dil and pinacidil used in angina.
Mechanism of actions
Potassium channel are known to play an important role in the regulation of membrane potential and excitability of cells. Potassium channel activators (K CHA) combine with ATP modulated potassium channels; opening these channels causes potassium ions to leak out from the cell and hyperpolarises the cell membrane of the vascular smooth muscle this is accompanied by relaxation of vascular smooth muscle. Thus, they act as direct arterial vasodilators.
Potential Clinical Applications of K Channel Openers
- Angina pectoris 2. Hypertension 3. Congestive Heart Failure 4. Myocardial salvage in MI 5. Antihypoglycaemic (Insulinoma) 6. Alopecia 7. Bronchial asthma 8. Urinary urge incontinence.
Management of Angina Pectoris
- Arrangement of life so as to reduce the number of attacks as far as possible. Weight reduction is helpful.
- Nitroglycerin to be taken before exercise that is expected to induce angina. It is also used to relieve the attack.
- The long-acting organic nitrates may be used for prophylaxis.
- Severe angina, unresponsive to drug treatment is an indication for surgical bypass grafting of the affected coronary arteries. Its role regarding the prognosis of such patients is controversial.
