Explain the pakinsonism disease. Anti- parkinsonism drugs.
Parkinson’s disease also known as PD is a degenerative disorder of the (CNS) central nervous system that often a the sufferers motor skills speech and other functions.
Parkinson’s disease belong to a group of conditions called movement disorders it is characterised by muscle rigidity tremor slowing of physical movement and in extreme case a loose or physical movement akinesia the commonly symptoms are the results of declared stimulation of the motor cortex by the basal ganglia normally caused by the insufficient formulation of dopamine which is producess in the dopaminergic neurones of the brain.
Secondary symptoms may include high level cognitive dysfunction and subtle language problem. PD is both chronic and progressive.
Sign and symptoms
Parkinson’s disease affects a movement producing motors symptoms non motor symptoms which include autonomic dysfunctions cognitive and neurobehavioral problems and century and sleep difficulties are also common but are under appreciated..
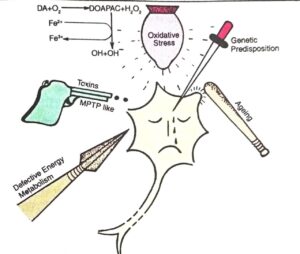
Causes
The most people with Parkinson’s disease are described as having idiopathic Parkinson’s disease having no specific known cause there are far less common causes of Parkinson’s disease including genetic toxins head tumor cerebral anoxia and drug induced parkinsonism disease.
Pathophysiology
The symptoms of Parkinson’s disease result from the greatly reduced activity of pigment dopamine secreting (dopaminergic )cells in the parts compact region of the substantia nigra literary black substance. These neurones project to the striatum and their loss leads to iteration in the activity of the neural circuits within the basal ganglia that regulate movement in essence inhibin station of the direct pathway and excitation of the indirect pathway.
The direct pathway facilitated movement it and the indirect pathway in a b movement the lake of dopamine results in decreased innervation of the ventral area nucleus of the thalamus which sends excitatory projections to the motor cortex thugs leading to hypo kinesia.
There are four major dopamine bath was in the brain the negrostriatal pathway, referred to above meditates movements and the most conspicuously affected in early Parkinson’s disease the other pathway are the mesocortical the mesolimbic and the tuberoinfundibular. Disruption of dopamine along the non striatal pathway likely explains much of the neuropsychtric pathology associated with Parkinson disease.
The mechanism by which the brain cells in Parkinson`s are lost may consist of an abnormal accumulation of the protein alpha- synuclein bound to ubiquitin complex cannot be directed to the proteosome. This protein accumulation forms proteinaceous cytoplasmic inclusions called lewy shown that the death of dopaminergic neurons by alpha-synuclein is due to adefact in the machinery that transports proteins between the endoplasmic reticulam (ER) and the Golgi apparatus. Certain protein like Rab 1 may reverse this defact caused by alpha- synuclein in animal models.
ANTI- PARKINSONIAN DRUGS
Drugs used in the treatment of parkinsonism.
1]. Drugs affecting brain dopaminergic system.
- Dopamine precursor :- Livodopa (l-dopa)
- Peripheral decarboxylase inhibitors.
- Carbidopa
- Benserazide
- Dopaminergic agonists
- Bromocriptine
- Pergolide
- MAO- B inhibitor
Selegiline
- COMT inhibitors
- Entacapone
- Tolcapone
- Dopamine facilitator
Amantadine.
2]. Drugs affecting brain cholinergic system.
- Central anticholinergic
- trihexyphenidyl
- procyclidine
- biperiden
- Anti histaminics
- Orphenadrine
- promethazine.
Drugs affecting brain dopaminergic system.
A.Dopamine precursor.
- Levodopa :- parkinsonism is a dopamine deficiency disease it is the most effective agent in the treatment of parkinsonism dopamine reduces hypokinesia and rigidity and sometimes benefit tremor.
Pharmacokinetics
Dopamine is not well absorbed from the gut and does not penetrate the CNS levodopa is absorbed from small intestine by active transport really crosses the blood brain barrier and is converted to dopamine.
Bioavailability of levodopa is affected by:
- Gastric emptying
If slow, levodopa is exposed to degrading enzymes present in gut wall and liver for a longer time less is available to penetrate blood brain barrier.
Adverse effects :-
Side effects of levodopa include loss of appetite ,agitation, insomnia, tachycardia, arrhythmical; total immobility at high levodopa blood levels may occur.
B. Peripheral decarboxylase inhibitors
Carbidopa and benserazide
These are dopa decarboxylase inhibitors which prevent the extracerebral breakdown of levodopa only and do not enter the CNS. Levodopa 250 mg plus 25 mg carbidopa or 100 mg levodopa plus 25 mg benserazide are recommended.
C. Dopaminergic agonists
The DA agonists can act on strudel DA receptors even in advanced patients who have largely lost the capacity to synthesize, store and release DA from levodopa.
- Bromocriptine:- It is an ergot derivative which acts as potent agonist on D2, but as partial agonist or antagonist on Dl receptors. Improvement in parkinsonism symptoms occurs within 1/2-1 hr of an oral dose of bromocriptine; and lasts 6-10 hours.
D. MAO-B inhibitor
- Selegiline (Deprenyl)
Monoamine oxidase-B inhibitor selegiline inhibits intracerebral metabolic degradation of dopamine. This results in the preservation of dopamine at the basal ganglia. Thus it enhances the therapeutic effect of levodopa and, dose of levodopa can be reduced. But this effect is brief.
E. coMT inhibitors
When peripheral decarboxylation of levodopa is blocked by carbidopa/benserazide, it is mainly metabolized by COMT to 3-O-methyldopa.
Entacapone
200 mg dose of l-dopa- carbidopa.
Tolcapone: 100-200 mg BD or TDS.
Adverse effect :- Adverse effects such as nausea, vomiting, dyskinesia, postural hypotension, hallucinations, etc.
F. Dopamine facilitator
- Amantidine
- This agent has been found to relieve akinesia, rigidity and tremor in parkinsonism.
- It acts by liberating dopamine from the residual intactnerve endings.
- The drug is absorbed orally and is excreted unchangedin urine
- It is administered in the dose of 100 mg per day increased to 100 mg twice a day after 7-10 days.
Adverse effect
These are generally not serious: insomnia, dizziness, confusion, nightmares, rarely hallucinations.
- Selegiline (Deprenyl) It is a selective MAO-B inhibitor. Two isoenzyme forms of MAO, termed MAO-A and MAO-B are recognized; the former predominating in peripheral adrenergic structures and intestinal mucosa, while the latter in the brain and blood platelets.
As an adjuvant to levodopa, it is beneficial in 50–70% patients and permits 20-30% reduction in levodopa dose.
Adverse effects Postural hypotension, nausea, confusion, accentuation of levodopa induced psychosis. Contraindicated in patients with convulsive disorders.
Interacts with pethidine: excitement, hyperthermia, respiratory depression.
SELMAX, SELGIN 5 mg tab; dose: 5 mg with breakfast and with lunch, either alone (in early cases) or with levodopa.
Central anticholinergics
In addition, certain H, antihistaminics have significant central anticholinergic property. There is little to choose clinically between these drugs, though individual preferences vary. All produce 10–25% improvement in clinical features, lasting 4-8 hours after a single dose.
They are the only drugs effective in drug (phenothiazine) induced parkinsonism. The antihistaminics are less effi’cacious than anticholinergics but are better tolerated by older patients. Their sedative action also helps. Orphenadrine has mild euphoriant action.
- Trihexyphenidyl (benzhexol); 2-12 mg/day, PACITANE, PARBENZ 2
- Procyclidine: 5-20 ing/day; KEMADRIN 25,5 mg tab
- Biperiden: 2-10 mg/day oral, im Oliv: DYSKINON 2 mg tab., 5 ing/in inj.
- Benztopine: 1-6 mg/day oral, im oriv.
- Orphenadrine: 100-300 mg/day DISPAL 50 mg tab
6.Premeibuzne: 25-75 mg/day: PHENERGAN 10,25 mg mg tab.
Some general points
- None of the above drugs alter the basic pathology of parkinsonism — the disease continues to progress. Considering that oxidative metabolism of DA generates free radicals which may rather hasten degeneration of nigrostriatal neurones, it has been argued that levodopa therapy might accelerate progression of parkinson’s disease.
- Selegiline may also be combined with levodopa during the deterioration phase of therapy to overcome ‘wearing off effect.
- Combination of levodopa with a decarboxylase inhibitor is the standard therapy for most patients. Slow and careful initiation over 2–3 months, increasing the dose as tolerance toearly side effects develops and then maintenance at this titrated level with frequent evaluation gives the best results.
- Abnormal movements appear, mostly conciding with the peak of levodopa action after each dose.
